Understanding Bone Grafting Materials for Implants & Bone Regeneration
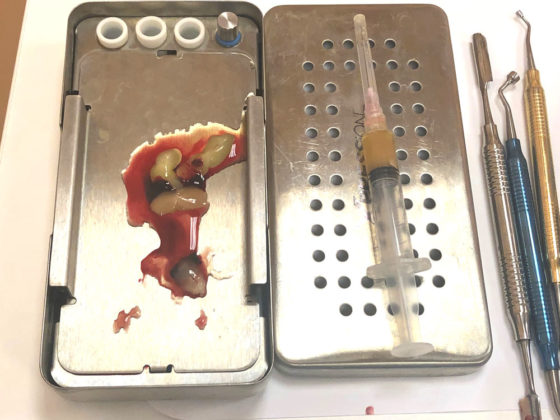
In some cases surgical procedures may require a bone grafting material used. We do not use bovine or cadaver bone. We can actually harvest your own biological material from your mandible. We also additionally harvest vials of blood which we spin. This creates a membrane out of your white stem cells and is known as LPRF.
LPRF and bone harvesting are used in some of the following ways:
- Guided bone regeneration (GBR)
- Guided tissue regeneration (GTR)
- Extraction Sockets
- Sinus Lift & Sinus Perforation
- Jaw Ridge Augmentation & Grafting (Ridge Split)
- Ceramic implant placement
Platelet Rich Fibrin (PRF)
PRF is 100% autogenous (meaning it comes from the patients’ own body) and is derived 100% from the patient’s blood. Outside of PRF, no other grafting material can govern and stimulate all 3 of the key processes involved in tissue and bone regeneration including angiogenesis, chemotaxis and cell proliferation. To this date, no exogenic agent can effectively govern all these processes, clearly highlighting PRF’s superior properties. It is estimated that less than 10% of dentists the USA use PRF for grafting and most instead choose to use allograft or other non-autologous bone grafting materials. Dr Litano is one of the few dental implant specialists in St Petersburg, Florida using platelet-rich fibrin therapy for dental implant placement and bone grafting, in addition of offering completely metal-free implants.
Why is Platelet Rich Therapy the Optimal in Bone Grafting & Tissue Regeneration?
Platelet rich therapy is the ultimate bioavailable therapy for stimulation and regeneration of cells in the body. While various growth factors are routinely used in reconstructive and regenerative therapies, the platelet rich fibrin therapy is the simplest and one of the most effective methods to extract growth factors from the blood’s platelets.
The Process of Platelet Rich Therapy and Blood work
Spinning to create L-PRF
Takes a blood draw from a patient and inserts the blood into a centrifuge to start the PRF procedures. The entire process takes approximately 20-30 minutes. PRF (platelet rich fibrin) is what is extracted from the blood cells using the centrifuge. After the initial blood draw from the patient, a platelet concentrate technique is applied through use of the centrifuge to separate the blood’s components, with the goal of increasing and concentraing the platelet count. The most essential component is the clotting because the platelets release their growth factors only after clotting, and it is after the growth factors are created that their use can be determined.
PRF
In PRF, the white cells are in the bottom of the clot. If blood is spun a high G force, valuable cells can be destroyed and to preserve the cells, Dr Litano spins the blood cells using a reduced RPM (revolutions per minute) and lower G force, to maximize the cell count and usage of the blood cells.
iPRF: Injectable-PRF (i-PRF) is the injectable version of PRF, which is liquid. i-PRF is made slightly differently, with an even lower G force, of 60 only (vs 200 for A-PRF) — followed by the same protocol, with no additive and no anticoagulant. The goal of i-PRF is to create a formation of a high concentration of white cells, plus fibrinogen, plasma protein have it clots spontaneously after the injection. Nothing additional needs to be added into the injection site to get the clot and to get the platelet to release growth factors. Injectable-PRF can be created by spinning for only three minutes. Spinning for four minutes will reduce the quality while increasing the liquid content and is generally suboptimal. The best concentration of the stem cells is spinning only for three minutes. More blood can be used to create more liquid.
Cell biology and the creation of collagen
Both plasma protein and white cells are necessary to create collagen synthesis, as white cells stimulate the inflammation response needed to draw fresh blood flow to the treatment area to create vascularization. At an injury site, the endothelial cells immediately separate themselves and then the white cells squeeze through the gaps and then by chemotaxis they move through the injury site, and begin to release the pro-inflammatory interleukins. This is the sort of inflammation that causes activation of monocytes into macrophages. The macrophages then dominate the inflammatory phase, and then they start to release growth factors and BNPS. Stem cells are necessary alongside white cells in order to achieve a smart blood concentrate and regenerate new tissue. White cells influence the quality of the PRP, so enriching the PRP with white cells creates greater tissue augmentation and a significantly higher proliferation of mesenchymal stem cells.
Bone Grafting Materials
Autograft: Recipient’s Own Bone
Autograft is obtaining of bone from the patient’s own body and typically is the gold standard grafting procedure available now.
Concerns: Autograft has its limitations, which include potential problems such as second surgical site and patient discomfort in terms of harvesting of a graft from another part of the patients body. It’s also a painful, complex and costly procedure for the patient.